Uterine Prolapse
Uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken until they no longer provide enough support for the uterus. As a result, the uterus slips down into or protrudes out of the vagina.
Uterine prolapse most often affects people after menopause who've had one or more vaginal deliveries, however it can happen at any age.
Mild uterine prolapse usually doesn't require treatment. But uterine prolapse that causes discomfort or disrupts daily life might benefit from treatment.
Symptoms
Mild uterine prolapse is common after childbirth. It generally doesn't cause symptoms. Symptoms of moderate to severe uterine prolapse include:
- Seeing or feeling tissue bulge out of the vagina
- Feeling heaviness or pulling in the pelvis
- Feeling like the bladder doesn't empty all the way when you use the bathroom
- Problems with leaking urine, also called incontinence
- Trouble having a bowel movement and needing to press the vagina with your fingers to help have a bowel movement
- Feeling as if you're sitting on a small ball
- Feeling as if you have vaginal tissue rubbing on clothing
- Pressure or discomfort in the pelvis or low back
- Sexual concerns, such as feeling as though the vaginal tissue is loose
Surgical Treatment
The goal of surgery is to repair your body and improve symptoms. Surgery can be performed through the vagina or the abdomen. There are several ways the surgery can be done, they include:
- Laparoscopic - the doctor places surgical instruments through the abdominal wall
- Robot-assisted surgery - robotic instruments are placed through the abdominal wall. They are attached to robotic arms, and are controlled by the surgeon.
Surgery is performed with native tissue repair, meaning that I use your own tissue to lift the uterus back up into the pelvis and secure it there.

Uterine Fibroids
Uterine fibroids are common non-cancerous growths of muscle that form within the muscular wall of the uterus (womb). Fibroids occur in up to 7 out of 10 women by the time they are aged 50.
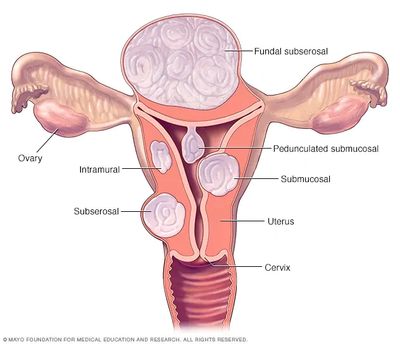
Fibroids (also known as uterine fibromyomas, leiomyomas or myomas) may grow in different layers of the uterus.
Fibroids can be located within the muscle (intramural); other types grow in the outer muscle layer (subserosal) or are inside the cavity of the uterus (submucosal).
Fibroids can vary in size, ranging from the size of a pea to the size of a rock melon or larger.
Most women have fibroids that don’t cause any symptoms. However, if fibroids cause problems, symptoms will depend on the size, number and location of the fibroids.
These may include the following:
- heavy or prolonged periods
- painful periods
- anaemia or iron deficiency (due to heavy periods), and you may feel:
- tired
- dizzy
- frequent passing of urine
- a pressure sensation on the bladder, bowel or back and/or feeling of incomplete emptying of bladder or bowel
- lower back pain
- swelling in the abdomen
- painful intercourse (dyspareunia)
Bleeding in between periods is not common but can sometimes happen. In rare instances, a fibroid may become cancerous and this is called a sarcoma.
A diagnosis of fibroids may be made during a vaginal examination, ultrasound or during surgery for other conditions.
The first test recommended is a transvaginal ultrasound, where the ultrasound probe is gently placed in the vagina. This is more accurate than a pelvic ultrasound where the probe is moved over the tummy (abdomen). Other tests may include MRI (magnetic resonance imaging).
Fibroids may be confirmed during a hysteroscopy, which is a procedure performed under local or general anaesthesia. A hysteroscope (a thin telescope) is carefully inserted along the vagina into a woman's uterus to examine the inside cavity.
Fibroids can also be confirmed during laparoscopy (keyhole surgery). This is an examination using a thin telescope, performed under general anaesthesia. Through small cuts in the abdomen, the doctor is able to look at or operate on the pelvic organs, such as the uterus, ovaries and fallopian tubes.
Medical Treatment Options:
- pain relief, including anti-inflammatory medications
- Tranexamic acid - a medication that reduces heaviness of bleeding by slowing blood clot breakdown in the uterine lining
- Mirena IUD - this T-shaped, contraceptive device is inserted into the uterus, and slowly releases a hormone called a progesterone, thereby reducing heavy bleeding
- Combined oral contraceptive pill - may reduce bleeding
- GnRH agonist - an artificial hormone used to prevent natural ovulation. May be used to shrink fibroid before a planned operation. Not recommended for longer term use because of side effects such as osteoporosis (bone thinning), and fibroid regrowth when the treatment is stopped.
- Iron replacement - either by oral tablets or an intravenous infusion
Surgical Treatment Options:
- Uterine artery embolisation (UAE) - small, sterile particles are injected into the uterine artery to reduce the blood supply to the fibroid, under sedation or general anaesthesia. This can make the fibroid shrink by a third or half its size.
- Hysteroscopic myomectomy - A hysteroscope is used under general anaesthesia to cut out a submucosal fibroid that is partially or completely inside the cavity of the uterus
- Myomectomy - a surgical procedure performed either laparoscopically or robotically to remove the fibroid
- Hysterectomy - removal of the uterus, either laparoscopically or robotically
Uterus with large fibroid, following hysterectomy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.